The usefulness of MRI for lung cancer is presented in Table 4.
After a report by Webb et al. of Radiologic Diagnostic Oncology Group of 1991, the Japanese guidelines for the use of MRI for lung cancer was restrictive for many years only being used in mediastinum invasion, chest wall invasion or vessel invasion. Due to the fact that the diagnostic ability of MRI is the same as that of CT for the diagnosis of the T factor and N factor of lung cancer many doctors who were already familiar with CT were reluctant to adopt the use of MRI. With cost and radiation use becoming more of an issue over the years the Japanese guidelines for the use of MRI for lung cancer have changed drastically.
Table 4
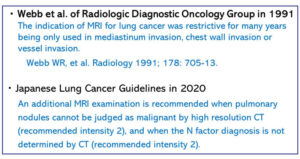
The Japanese Lung Cancer Guidelines for 2022 for MRI are shown in Table 4. An additional MRI examination is recommended when pulmonary nodules cannot be judged as malignant by high resolution CT, and when the N factor diagnosis is not determined by CT.
- Usefulness of MRI for diagnosis of pulmonary nodules and masses (PNMs)
Next two meta-analysis of MRI (DWI) reported that MRI (DWI) is useful for a differential diagnosis of benign and malignant PNMs (Table 5).
Li B, et al. A systematic review and meta-analysis of the accuracy of diffusion-weighted MRI in the detection of malignant pulmonary nodules and masses. Acad Radiol 2014; 21: 21-9.
Shen G, et al. Apparent diffusion coefficient values of diffusion-weighted imaging for distinguishing focal pulmonary lesions and characterizing the subtype of lung cancer: a meta-analysis. Eur Radiol 2016; 26: 556-66.
The next two papers mentioned that the diagnosability of MRI (DWI) is same or better than that of PET-CT (Table 2-2). Our results are presented in Table 5.
Mori T, et al. Diffusion-weighted magnetic resonance imaging for diagnosing malignant pulmonary nodules/masses: comparison with positron emission tomography. J Thorac Oncol 2008; 3: 358-364.
Usuda K, et al. Diagnostic performance of diffusion weighted imaging of malignant and benign pulmonary nodules and masses: comparison with positron emission tomography. Asian Pac J Cancer Prev. 2014; 15 (11):4629-4635.
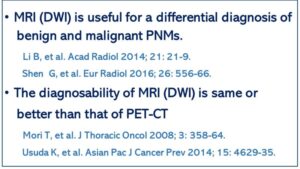 Table 5 Pulmonary nodules and masses (PNMs) Comparison between MRI and PET-CT
Table 5 Pulmonary nodules and masses (PNMs) Comparison between MRI and PET-CT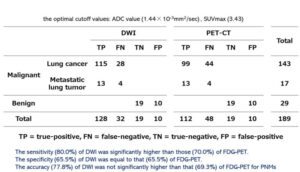 Table 6 Comparison of DWI and PET-CT in malignant and benign pulmonary nodules and masses (PNMs) Usuda K, et al. Asian Pac J Cancer Prev 2014; 15: 4629-35.
Table 6 Comparison of DWI and PET-CT in malignant and benign pulmonary nodules and masses (PNMs) Usuda K, et al. Asian Pac J Cancer Prev 2014; 15: 4629-35.
- Usefulness of MRI (DWI) for lung cancer clinical staging
Here are some radiological images of three cases of lung cancers in Fig.7-11. In case 1, an adenocarcinoma shows a nodular mass in CT, an FDG accumulation in PET-CT and a decreased diffusion in MRI (DWI). The adenocarcinoma had a metastasis of the #12u lymph node pathologically. In case 2, an adenocarcinoma did not have FDG accumulation of #12L lymph node, but diffusion decrease of the #12u lymph node. Pathological positive lymph node metastasis revealed that MRI (DWI) showed the correct diagnosis. In case 3, a large cell carcinoma had FDG accumulation of #4L lymph node, but no diffusion decreases of the #4L lymph node. Pathological positive lymph node metastasis revealed MRI (DWI) showed the correct diagnosis.
Usuda K, et al. Advantages of diffusion-weighted imaging over positron emission tomography-computed tomography in assessment of hilar and mediastinal lymph node in lung cancer. Ann Surg Oncol 20; 1676-1683: 2013.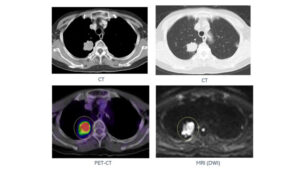 Fig. 7 Case 1. Adenocarcinoma
Fig. 7 Case 1. Adenocarcinoma
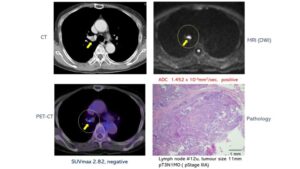 Fig. 8 Case 1. Adenocarcinoma. PET-CT showed
Fig. 8 Case 1. Adenocarcinoma. PET-CT showed
the #12u was negative but MRI (DWI) showed the #12u was positive. The adenocarcinoma had a metastasis of the #12u lymph node pathologically.
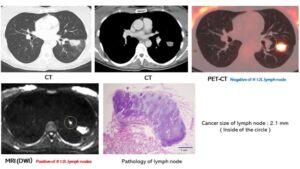 Fig. 9 Case 2. An adenocarcinoma did not have FDG accumulation of #12L lymph node, but diffusion decrease of the #12u lymph node. Pathological positive lymph node metastasis revealed MRI (DWI) showed correct diagnosis. Usuda K, et al. Ann Surg Oncol 2013; 20: 1676-83.
Fig. 9 Case 2. An adenocarcinoma did not have FDG accumulation of #12L lymph node, but diffusion decrease of the #12u lymph node. Pathological positive lymph node metastasis revealed MRI (DWI) showed correct diagnosis. Usuda K, et al. Ann Surg Oncol 2013; 20: 1676-83.
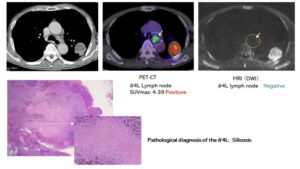 Fig. 10 Case 3. A large cell carcinoma had FDG accumulation of #4L lymph node, but no diffusion decrease of the #4L lymph node. Pathological positive lymph node metastasis revealed MRI (DWI) showed correct diagnosis. Usuda K, et al. Ann Surg Oncol 2013; 20: 1676-83.
Fig. 10 Case 3. A large cell carcinoma had FDG accumulation of #4L lymph node, but no diffusion decrease of the #4L lymph node. Pathological positive lymph node metastasis revealed MRI (DWI) showed correct diagnosis. Usuda K, et al. Ann Surg Oncol 2013; 20: 1676-83.
The size of metastatic lymph nodes detected by MRI (DWI) or PET-CT are shown in Fig. 11. MRI (DWI) can detect smaller metastatic lymph nodes. The average value of the maximum diameter of carcinomas in metastatic lymph node stations was not detected by either DWI or PET-CT (A), was detected by DWI (B), and was detected by PET-CT (C). The maximum diameter of carcinomas in metastatic lymph node stations were 3.0 ±0.9 mm in A, 7.2 ±4.1 mm in B, and 11.9 ±4.1 mm in C. There were significant differences among the groups.
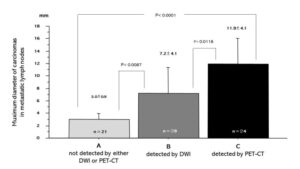 Fig.11 The average value of maximum diameter of carcinomas in metastatic lymph node stations not detected by either DWI or PET-CT (A), detected by DWI (B), and detected by PET-CT (C).
Fig.11 The average value of maximum diameter of carcinomas in metastatic lymph node stations not detected by either DWI or PET-CT (A), detected by DWI (B), and detected by PET-CT (C).
Muximum diameter of carcinomas in metastatic lymph node stations were 3.0 ±0.9 mm in A, 7.2 ±4.1 mm in B, and 11.9 ±4.1 mm in C. There were significant differences among groups. Usuda K, et al. Ann Surg Oncol 2013; 20: 1676-83.
A comparison between MRI (DWI) and PET-CT for lymph node metastases of lung cancer (Table 12).
Peerlings et al. reported that the sensitivity of MRI (DWI) for metastatic lymph nodes of lung cancer was 0.87 and the specificity of MRI (DWI) for no metastatic lymph nodes of lung cancer was 0.88.
Peerlings J, et al. The diagnostic value of MR imaging in determining the lymph node status of patients with non-small cell lung cancer: a meta-analysis. Radiology 2016; 281: 86-98.
Shen et al. concluded that an assessment of MRI (DWI) was useful for N factor of lung cancer.
Shen G, et al. Performance of DWI in the nodal characterization and assessment of lung cancer: a meta-analysis. AJR Am J Roentgenol 2016; 206: 283-290.
Our article which dealt with 160 lung cancer patients showed that the accuracy of MRI(DWI)was 96.2%, which was significantly better than that of (94.3%) of PET-CT.
Usuda K, et al. Advantages of diffusion-weighted imaging over positron emission tomography-computed tomography in assessment of hilar and mediastinal lymph node in lung cancer. Ann Surg Oncol 20; 1676-1683: 2013.
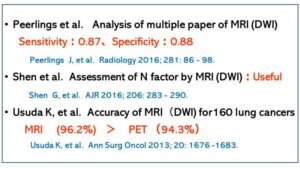
Table 12 A comparison between MRI (DWI) and PET-CT for lymph node metastases of lung cancer
The sensitivity and the accuracy of metastatic lymph nodes
Concerning advantages of MRI (DWI), sensitivity and accuracy of MRI (DWI) are significantly higher than those of PET-CT (Table 13).
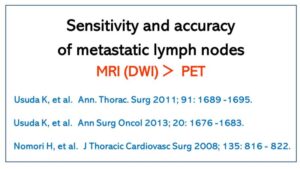
Table 13 Advantages of MRI (DWI)
Usuda K, et al. Advantages of diffusion-weighted imaging over positron emission tomography-computed tomography in assessment of hilar and mediastinal lymph node in lung cancer. Ann Surg Oncol 20; 1676-1683: 2013.
Usuda K, et al. Diffusion-weighted imaging is superior to PET in the detection and nodal assessment of lung cancers. Ann. Thorac. Surg. 91(6): 1689-1695, 2011.
Usuda K, et al. Diagnostic Performance of Diffusion Weighted Imaging for Multiple Hilar and Mediastinal Lymph Nodes with FDG Accumulation. Asian Pac. J. Cancer Prev. 16, 6401-6406, 2015.
- Usefulness of MRI for the invasion into blood vessels, heart, chest wall, diaphragm and the mediastinum by lung cancer
This fact has been well known for more than 30 years. The evaluation, by MRI, for the invasion into blood vessel, heart, chest wall, diaphragm and the mediastinum by lung cancer is the gold standard. For this evaluation CT or PET-CT is not reliable enough.
- MRI (DWI) is valuable for the evaluation of lung cancer with multiple FDG accumulation in PET-CT (Fig. 14, Table 15).
MRI (DWI) is valuable for an evaluation of lymph nodes affected by pneumoconiosis or silicosis. MRI (DWI) can judge the FDG accumulation of pneumoconiosis as negative.
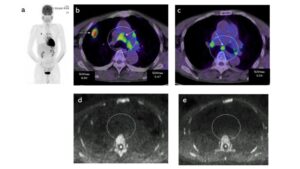
Fig. 14 Usefulness of MRI (DWI) in a lung cancer with FDG accumulation of multiple lymph nodes. A squamous cell carcinoma, but without lymph node metastasis. The patient was diagnosed as N2 disease by PET-CT, but N0 disease by DWI. DWI showed lymph node station #4R as negative (d), and lymph node station #7 as negative (e). The lymph nodes were diagnosed as pneumoconiosis pathologically. Usuda K, et al. Asian Pac. J. Cancer Prev. 2015:16: 6401-6406.
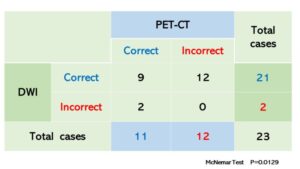 Table 15 Comparison of accuracy between DWI and PET-CT for lung cancer with FDG accumulation of multiple lymph nodes Usuda K, et al. Asian Pac. J. Cancer Prev. 16, 6401-6406, 2015.
Table 15 Comparison of accuracy between DWI and PET-CT for lung cancer with FDG accumulation of multiple lymph nodes Usuda K, et al. Asian Pac. J. Cancer Prev. 16, 6401-6406, 2015.
Usuda K, et al. Diagnostic Performance of Diffusion Weighted Imaging for Multiple Hilar and Mediastinal Lymph Nodes with FDG Accumulation. Asian Pac. J. Cancer Prev. 2015; 16: 6401-6406.
- Usefulness of the MRI (DWI) for detecting metastatic or recurrent lesions of lung cancer
The detection of metastatic or recurrent lesions is easy based on the diffusion decrease by the MRI (DWI) and a qualitative diagnosis can be possible by measuring ADC.
Usuda K, et al. Recurrence and metastasis of lung cancer demonstrate decreased diffusion on diffusion-weighted magnetic resonance imaging. Asian Pac J Cancer Prev. 15; 6843-6848, 2014.
- Diffusion-weighted whole-body imaging with background suppression (DWIBS) (Whole-body DWI)
The research group of Professor Dr. Taro Takahara and Professor Dr. Yutaka Imai of Tokai University have developed an epoch-making method, diffusion-weighted whole-body imaging with background suppression (DWIBS) which searched a whole body with one MRI (DWI) exploration in 2004. The diagnostic ability of PET-CT and that of DWIBS are similar. Some diagnostic abilities are better in DWIBS than in PET-CT, others are better in PET-CT than DWIBS. However, patients cannot receive a PET-CT more than once a year on health insurance because it is expensive, approximately ¥30,000 (30,000 JPY) with a 30% deductible. On the other hand, DWIBS is an MR imaging so we do not need a contrast medium. Therefore, a patient can get an MRI once every one to three months on health insurance.
We present the good points of DWIBS compared to PET-CT (Table 16). Also, we show a comparison between DWIBS and PET-CT (Table 17).
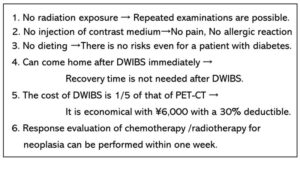 Table 16 Advantages of DWIBS compared with PET-CT
Table 16 Advantages of DWIBS compared with PET-CT
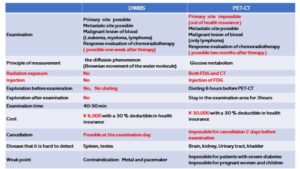
Table 2-9 Comparison between DWIBS and PET-CT